Living Donor Liver Transplant
What is living donor liver transplant (LDLT)?
Living donor liver transplant (LDLT) is an important life-saving procedure for patients suffering from decompensated liver cirrhosis, acute liver failure and hepatocellular carcinoma (HCC) (liver cancer).
It can be performed on patients with end-stage liver disease regardless of the original cause of the disease. Potential recipients are carefully selected and must meet stringent criteria.
LDLT offers many advantages over cadaveric liver transplantation:
- Surgery can be scheduled when the recipient's condition is optimised.
- The quality of the liver graft is better because it is provided by a healthy donor, with a shorter cold ischaemic time (the time the donated liver has no blood supply).
- Waiting time for LDLT is much shorter than cadaveric liver transplant, which is very important for patients with rapidly progressive liver diseases or deteriorating liver function, or both.
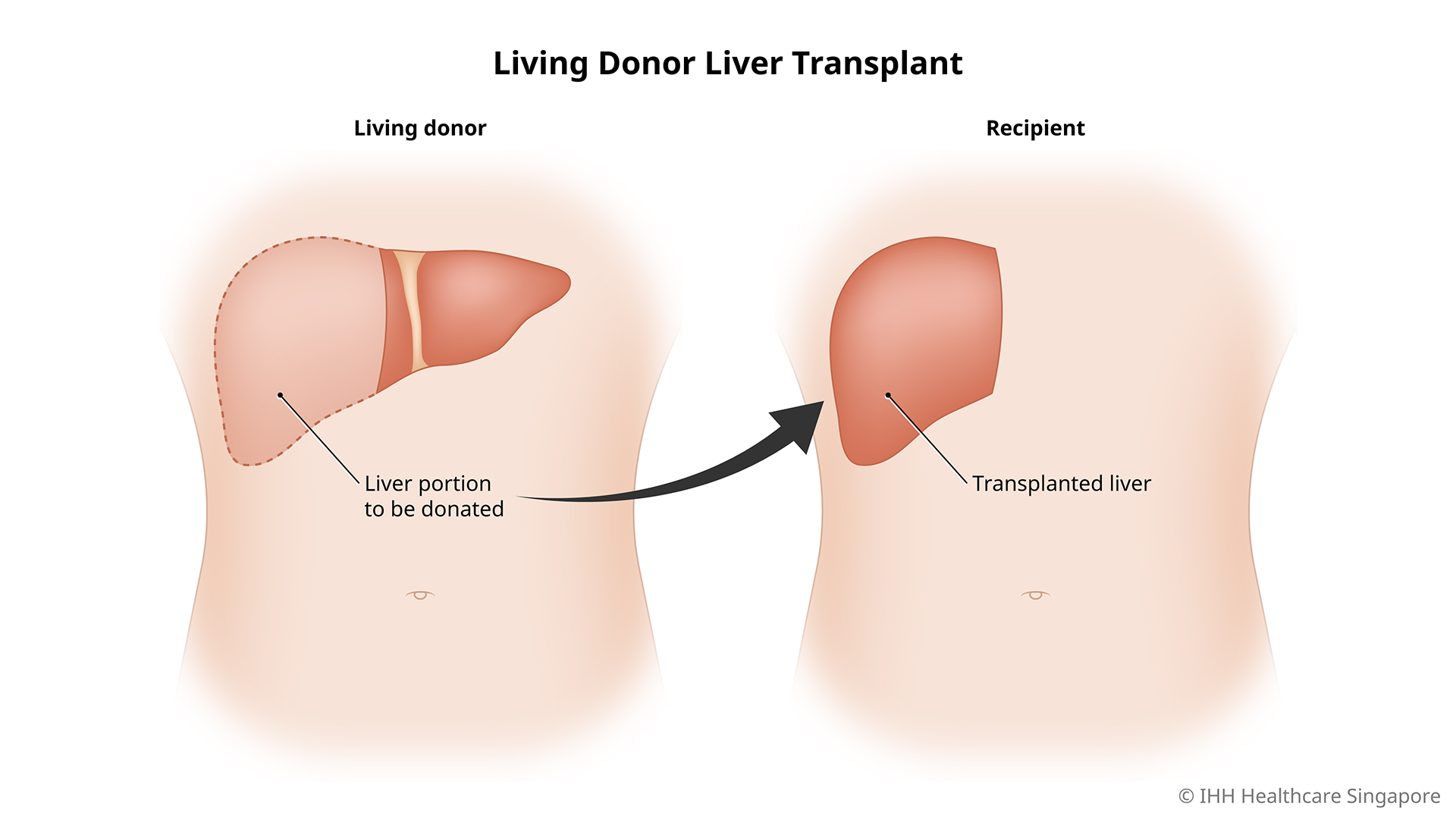
How it works
In LDLT, a healthy donor donates part of their healthy liver to replace the damaged liver of the recipient.
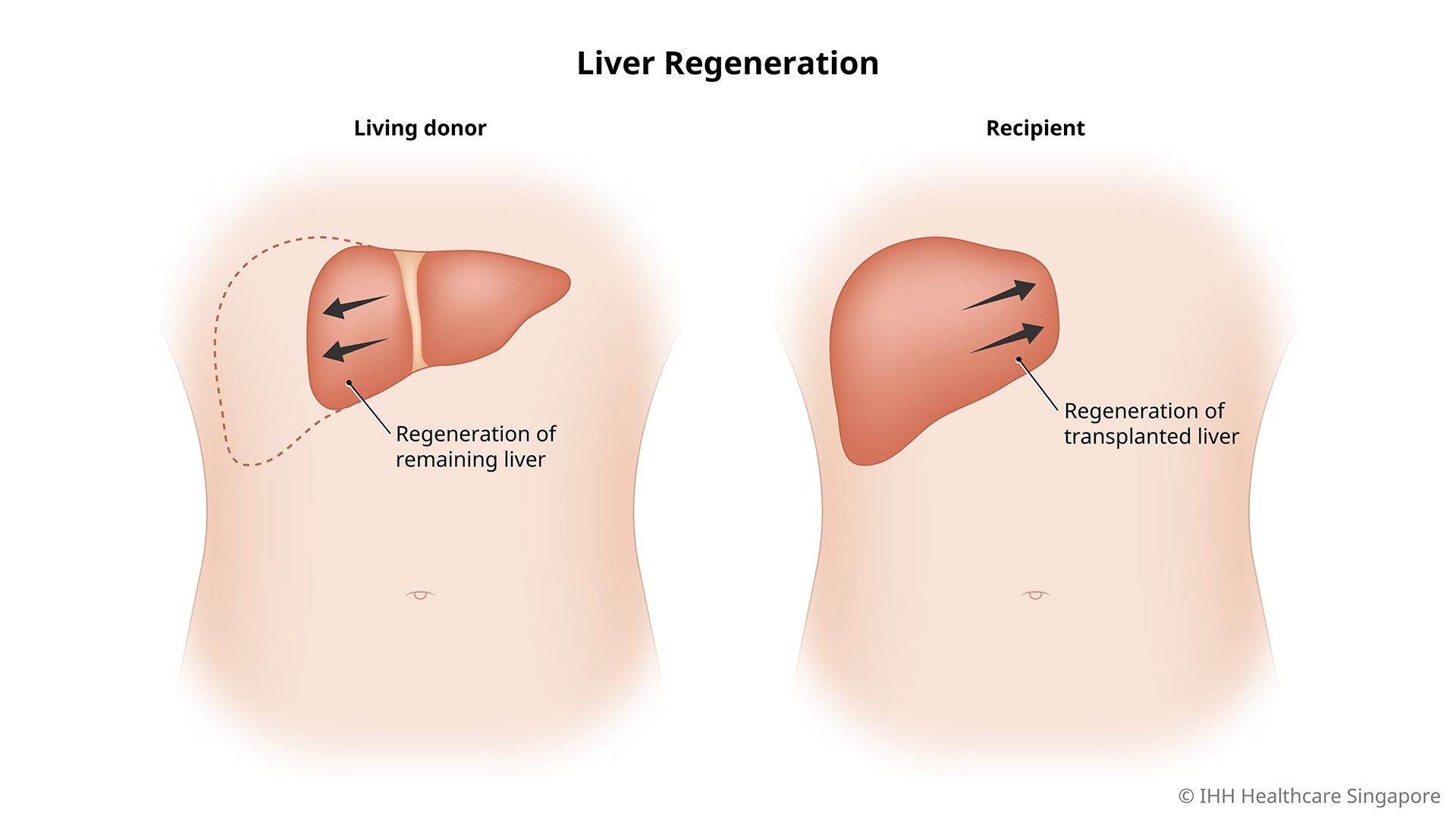
Both the transplanted liver and the portion left behind in the donor are able to regrow rapidly. Even with 70% of its mass removed, the liver will regenerate to 100% functionality within 4 – 6 weeks.
Living donor liver transplant requirements
A suitable living donor would meet the following requirements:
- Aged between 18 – 60
- Be of a healthy weight, in good health and psychologically sound
- Have a compatible blood type with the patient
- Have a healthy functioning liver and kidney
- Willing and prepared to go through the entire living donor liver transplant process including pre-donation evaluation, surgery and recovery
Why do you need an LDLT?
LDLT is usually a treatment for:
- Patients with end-stage liver disease.
- Decompensated liver cirrhosis (liver scarring) in adults. Liver cirrhosis is mainly caused by hepatitis B and C, chronic alcohol consumption, autoimmune liver disease and build-up of fat in the liver.
- Biliary atresia in children, caused by absent or blocked bile ducts, which are tubes that carry bile out of the liver to the gallbladder. The bile backs up and damages liver tissue, and eventually leads to cirrhosis.
Other reasons for LDLT include:
- Liver cancer
- Benign (non-cancerous) liver tumours
- Hereditary liver diseases
Who should not undergo an LDLT?
Liver transplant is recommended only when the risk of demise from the liver disease outweighs the immediate and long-term risks of the transplant. You may not be suitable for liver transplant if you have:
- An active infection
- Cancer outside of the liver
- Alcohol or drug abuse
Your doctor will advise you on your suitability for a living donor liver transplant.
What are the risks of an LDLT?
Liver transplant surgery carries a risk of complications including:
- Bile duct complications, including bile duct leaks or strictures of the bile ducts
- Bleeding
- Blood clots
- Failure of donated liver
- Infection
- Rejection of donated liver
Long-term complications may also include recurrence of liver disease in the transplanted liver.
While the procedure is often life-saving for the recipient, donating a portion of the liver also carries certain risks for the donor. Some mild but uncommon complications that may occur for the donor include:
- Hernia at the incision site
- Prolonged numbness
- Wound infection
Severe complications are rare and the surgeon will discuss them in detail with you prior to the surgery.